At a community symposium on health care and homelessness attended by over 250 Londoners, a research team from Lawson Health Research Institute announced the results of a nine-month, federally funded project tackling the issue of homelessness from within hospital walls.
The No Fixed Address (NFA) strategy reaches and supports patients during the crucial transitional period when they are being discharged from the hospital and re-integrated into the community. The approach was initially tested with strong success for mental health patients across the city and the second ‘version’ of the project was extended to medical units at London Health Sciences Centre’s University Hospital and Victoria Hospital.

“Many of our patients with lived experience of homelessness were saying that their journey started with a hospital discharge,” explains Dr. Cheryl Forchuk, Assistant Scientific Director at Lawson and NFA project lead. “They were often experiencing major transitions in their lives and then experienced a hospital stay. Normally a relatively short visit, they aren’t able to gather the information and make a plan to be able to leave the hospital with somewhere to stay.”
Through partnerships between service providers and non-profit organizations, the NFA strategy helps prevent homelessness by providing timely and accessible supports to patients who would otherwise be discharged into homelessness. Staff from the Canadian Mental Health Association Middlesex, Salvation Army’s Housing Stability Bank, and Ontario Works in the City of London provided direct, on-site patient access to housing and income support databases
“Lawson’s No Fixed Address research project is the first evaluation anywhere of a strategy that aims to reduce the number of hospital patients being discharged into homelessness,” says Dr. Forchuk.
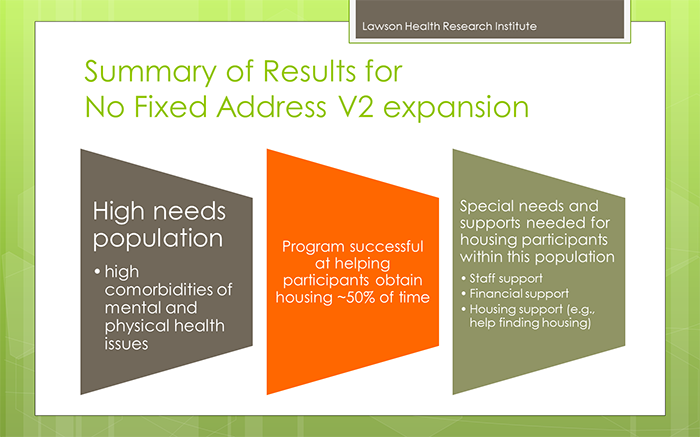
Over nine months, 74 people experiencing medical health issues accessed the NFA program. Of those, 54 per cent were also experiencing mental health challenges.
All of the study participants were in imminent danger of homelessness. Through the supports provided as part of this research study, half were able to arrange housing before being discharged.
“We were able to help a lot of people, with 50 per cent successfully securing housing,” shares Dr. Forchuk. “With the results and feedback we received, we learned a lot about how we can make the program even better.”
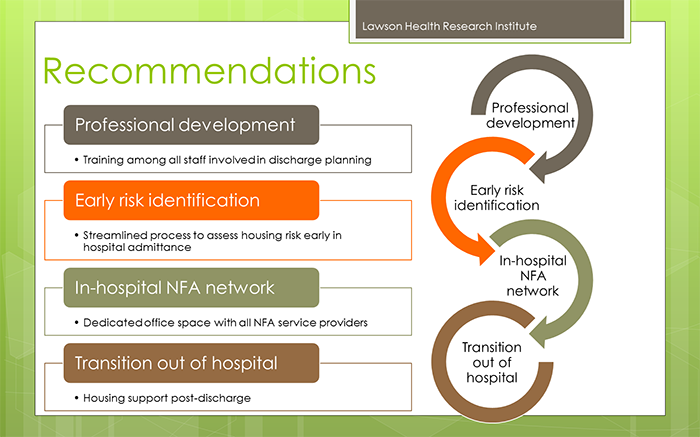
They found that there is a need for the supports to be extended as a transitional program in the community post-discharge, as the length of stay in the medical units tended to be short.
The project’s previous phase, involving acute and tertiary psychiatric care in the London region, prevented homelessness in 95 per cent of cases. “Going into the medical units, we found that people have highly complex needs that often involved mental health challenges.
By simply using the same approach that we did for those in psychiatric care, we helped half of the people find housing. To best serve the needs of everyone, we want to follow them after discharge.”
The team sees a solution in having a housing support worker provide transitional, wrap-around services that follow the person. They would continue to meet and work together after the hospital stay, helping to access community programs.
“This role would be embedded in both the health care system and the homeless serving system, supporting individuals who have complex physical and mental health issues as they are also navigating homeless resources.”
This project is funded by the Government of Canada's Homelessness Partnering Strategy’s (HPS) Innovative Solutions to Homelessness funding stream.