

The immune system is one of our greatest defenses against disease and injury. But what happens when it betrays us?
With conditions like rheumatoid arthritis the immune system is manipulated to attack the human body. Inflammation, normally a protective immune response, can be employed to cause symptoms like pain.
Surprisingly, research suggests our immune system may be similarly affected in patients with neurodegenerative dementias.
“We know there are increased numbers of inflammatory cells in the brains of patients with dementia but we don’t know what role they’re playing,” says Dr. Elizabeth Finger, a scientist at Lawson Health Research Institute and neurologist at St. Joseph’s Health Care London’s Parkwood Institute. “Are they doing their proper job of cleaning up damaged cells or is their presence more sinister?”
Dr. Finger’s research group aims to identify and understand changes in the brain that lead to symptoms of dementia, find novel treatments to improve patient quality of life and hopefully prevent the disease altogether. Critical to this work is Dr. Finger’s collaboration with Lawson Imaging scientists Drs. Keith St. Lawrence, Udunna Anazodo, and Justin Hicks.
The researchers utilize Canada’s first hybrid positron emission tomography and magnetic resonance imaging (PET/MRI) machine located at St. Joseph’s Hospital. This high-powered imaging allows them to assess changes to both structure and function in the brains of patients with neurodegenerative dementias like Alzheimer’s disease, frontotemporal dementia and Lewy body dementia.
In one of their many studies they are examining whether there is inflammation in the brains of patients with frontotemporal dementia and, if so, whether this inflammation is present in areas of the brain not yet damaged by the disease.
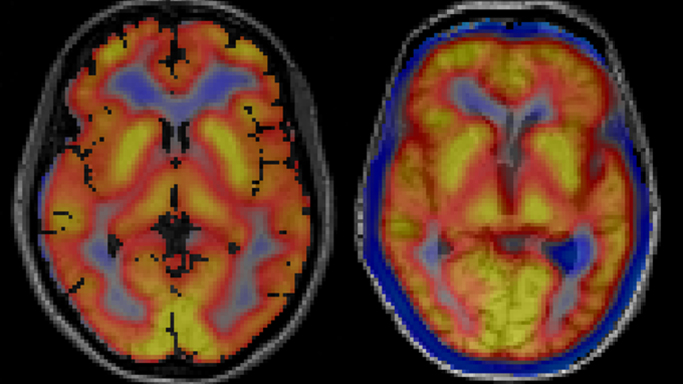
Images captured using a hybrid PET/MRI machine show activated immune cells in the frontal brain regions in a patient with frontotemporal dementia (right) compared to a healthy volunteer (left).
“A presence in those parts of the brain would suggest that inflammation is not playing its normal role of cleaning up damaged cells,” explains Dr. Finger. “It would suggest the brain’s immune response is overactive and that we should consider clinical trials for medications that modulate this response.”
Dr. Finger is an active investigator for novel therapies. In 2019, her group will participate in at least two clinical trials for medications that target genetic mutations that can cause frontotemporal dementia. The studies are phase I trials, which means they are the first time the medications are being tested in humans.
Dr. Finger is also leading a North American multi-centre trial called FOXY. The study will examine the therapeutic potential of a hormone called oxytocin to improve the loss of emotion and empathy that frequently occurs in patients with frontotemporal dementia.
“In the past there were very few treatments for frontotemporal dementia,” explains Dr. Finger. “We are glad to say that Lawson and St. Joseph’s will offer the opportunity to take part in these advances. Words cannot adequately express the appreciation we have for our patients, caregivers and healthy volunteers who participate in research. The time and effort they selflessly donate with the goal of helping future patients is truly inspiring and motivating.”
This story originally appeared in an annual publication from the Alzheimer Society London and Middlesex.